IPHA stands firm as payments to healthcare staff and organisations come under scrutiny again
By Chris Wheal
August 13, 2024
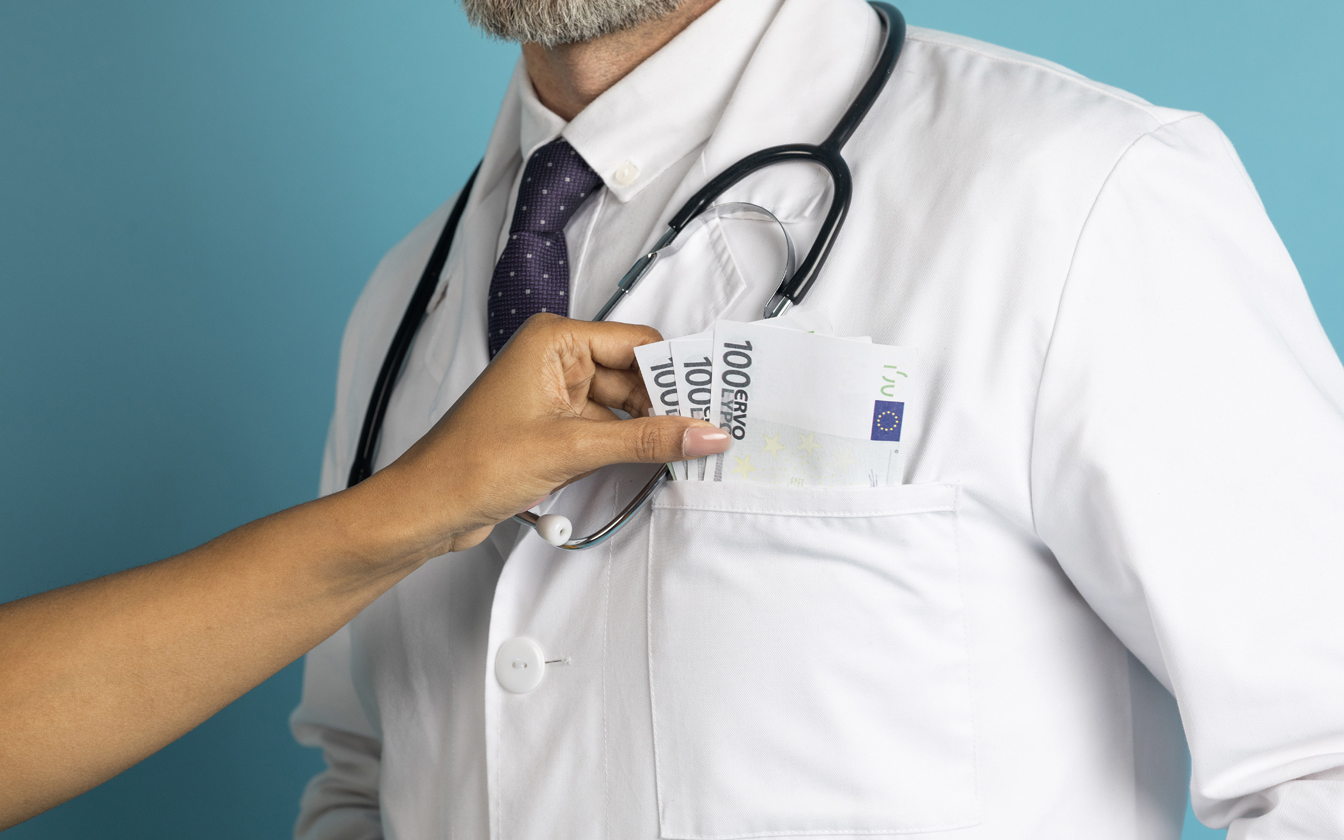
Allegations that pharma cash leads to "inappropriately increased prescribing rates, higher prescribing costs and lower prescribing quality".
The Irish Pharmaceutical Healthcare Association (IPHA) has defended its transparency reporting of how industry funds individual healthcare workers and their organisations.
Responding to calls for stronger legislation from Royal College of Surgeons pharmaceutical transparency campaigner James Larkin, the IPHA issued PharmaLifeScience with a robust defence.
Eimear O’Leary, IPHA director of communications and advocacy, said: “IPHA believes that voluntary disclosure codes that are well designed and consistently implemented are effective and more quickly adaptable to changing circumstances than primary legislation.
“IPHA engages with all stakeholders to support public disclosure and is strongly supported by the Health Service Executive (HSE), medical groups and learned societies. We are not aware of a significant gap in disclosure requirements that could not be filled using voluntary codes that apply to all marketing authorisation holders. Therefore, we are not aware of a clear rationale for the replacement of the IPHA voluntary code with legislation.”
Benefit to patients
O’Leary also highlighted the benefits of pharmaceutical firms working closely with healthcare professionals. “The shared ambition of IPHA member companies is to make available life-enhancing medicines, including vaccines, for patients in Ireland via those entitled to prescribe and supply. In relation to this, collaboration between industry and healthcare professionals benefits patients.
“It is a relationship that has helped deliver numerous life-enhancing medicines and changed the way many diseases impact on our lives,” she said.
Transfers of value
The IPHA announced its disclosure of how money and other forms of backing – called transfers of value (ToV) – get to healthcare professionals (HCPs) and healthcare organisations (HCOs). It has published the full database. The headline figures are:
· The total paid to individuals was €5,953,436 (compared with €4,647,825 in 2022). Some 96% of individual healthcare professionals are named and the IPHA says this transparency is a 17% improvement on 2022. The proportion of named individuals has increased year on year since the website first went live in 2016.
· The total paid to healthcare organisations was €8,892,758, which is a 4% decrease on 2022 data. All organisation transfers were disclosed individually.
· The total ToV amount for 2023 was €29,039,301 which is a 10% increase compared with 2022. However, that figure includes €14,193,107 in R&D investment in 2023, a 16% increase in R&D investment on the 2022 figure.
Royal College of Surgeons not happy
But Royal College of Surgeons pharmaceutical transparency campaigner James Larkin claimed the revelations did not go far enough. Larkin is a postdoctoral researcher focusing on pharmacy and biomolecular sciences in the Department of General Practice at the Royal College of Surgeons in Ireland (RCSI).
“It’s problematic that the level of payments overall is increasing given that receipt of payments from the pharmaceutical industry is associated with inappropriately increased prescribing rates, higher prescribing costs and lower prescribing quality,” Larkin told PharmaLifeScience.
“It’s positive that the level of disclosure for healthcare professionals is increasing. However, there still appear to be major shortcomings associated with this database that have not been solved since we pointed them out in 2021.”
Larking gave a list of problems he has with the IPHA database and said it was “a non-exhaustive list”:
· There is no disclosure of the identity of R&D payment recipients
· Several transfer of value types are not covered by the database, examples include share ownership
· Enforcement measures for the database are extremely limited
· Several companies that are not members of the IPHA do not report payments on transferofvalue.ie
· Unique identifiers are not consistently provided for recipients
· The database is not downloadable
Larkin demanded legislation to enforce better transparency. “In order to address these issues, the Irish government should pass the Healthcare Transparent Payments Bill 2022, which would create a mandatory database and address these issues as well as others,” he said.
Robust defence
IPHA’s O’Leary told PharmaLifeScience: “Since 2017, IPHA has worked to provide increasing transparency in the public reporting of transfers of value between companies and HCOs and HCPs.” She claimed that since 2017:
· The transfer of value platform has annual returns from over 47 companies, including non-IPHA members.
· 100% of transfers of value to HCOs are disclosed with named recipients.
· Within GDPR requirements, we have worked to drive towards full transparency of ToVs to HCPs. The rate of individual disclosure has risen from 64% in 2019 to 96% now (2023 data).
· The Royal College of Physicians in Ireland Guidelines note that “collaboration between industry and RCPI has the potential to deliver significant benefits and that industry plays a valid and important role in the provision of medical education. However, this relationship needs to be based on clear ethical principles and should be transparent”.
· In a letter from February 2023 the HSE stated how it strongly believes that any ToV received by an HSE employee / HSE healthcare professional should be disclosed on the ToV. The HSE would not, in general, support a request for non-disclosure. The HSE would, in addition to the above, flag that its distinct preference would be that an individual company should not repeat ToVs to any HSE-employed HCP who has refused to allow publication of a previous ToV received from that company unless exceptional circumstances apply.
Tackling Larkin’s specific criticisms, the IPHA said: “Disclosing information about R&D has the potential to compromise confidential information and breach competition laws.” It said R&D activities – and in particular clinical trials – are subject to further transparency legislation. This includes the:
· EU Clinical Trial Regulation (2001/20)
· European Medicines Agency Transparency Policy (Policy 0070)
· EU Clinical Trials Register and Innovative Medicines Initiative
The database is not downloadable for data protection reasons and this had the backing of the Data Protection Commission.
“According to the Data Protection Commission (DPC) opinion, the safeguards put in place by IPHA to implement the principles of data minimisation and to protect the fundamental rights of data subjects, and the implementation of protocols to protect the data from search engine indexing is particularly welcomed. This should ideally mean that the information will only be available to persons who seek to access it for legitimate purposes, and it will be protected from webscraping or other harmful practices,” O’Leary said.
European standards
The IPHA said its work was in line with European standards and often tougher than legislation. “It is important to note that the provision of support to HCPs is regulated by legislation and the industry self-regulatory code put in place by IPHA as part of the European Federation of Pharmaceutical Industries and Associations (EFPIA).
“This code reflects, and in some instances is more strict than, the legislation. It is a condition of membership of IPHA to adhere to the code, including its disciplinary procedures. While the Code and legislation permit the promotion of medicines to HCPs, there are strict controls around this activity. In particular, the interactions between our industry and HCPs must meet high standards of integrity and transparency.
“In addition to requiring our members to adhere to our self-regulatory code, regulatory inspections of compliance with the legislation by the Health Products Regulatory Authority (HPRA) are welcomed because they facilitate the development and improvement of high standards.”
Exchange of information
O’Leary told PharmaLifeScience the relationships between industry and healthcare professions were all about exchanging information and subject to strict rules on what could and could not be paid for.
“Activities can range from conducting clinical research to sharing best clinical practice and exchanging information on how new medicines fit into the patient pathway. In this respect, HCPs may receive support to attend educational meetings, such as congress registration fees, travel and accommodation.
“HCPs may also provide expertise and insight by attending advisory boards, speaking at education and training meetings or acting in a consultancy role,” she said.
Do payments to healthcare workers affect their prescribing?







.png)